DOSING & ADMINISTRATION
Are you a Healthcare Professional or a Patient or Care Partner?
DOSING & ADMINISTRATION
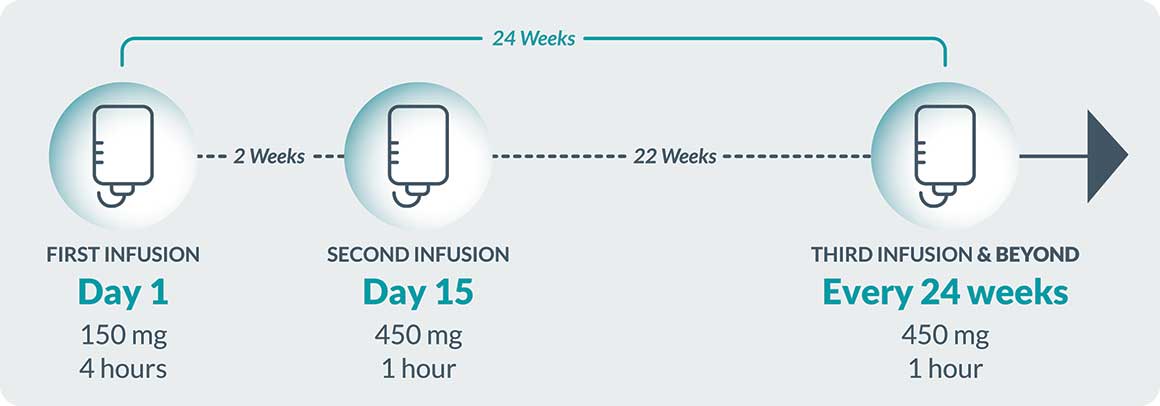
BRIUMVI is a 1-hour, 450 mg intravenous (IV) infusion given every 24 weeks following the starting dose1
95%
of all BRIUMVI infusions were completed in 1 hour without interruption in clinical trials*2
*± 5 minutes
After the third infusion and beyond, post-infusion monitoring is at physician discretion unless infusion reactions and/or hypersensitivity have been observed in association with the current or any prior infusion
DMT=Disease-modifying therapy
Assessments prior to the first dose of BRIUMVI1



Assessment before every infusion1


aWithdraw and discard the required volume of 0.9% sodium chloride injection, USP from the infusion bag following the preparation instructions
bInfusion duration may take longer if the infusion is interrupted or slowed.
cAdminister the first subsequent infusion 24 weeks after the first infusion.
Stop infusion immediately and permanently discontinue BRIUMVI. Provide appropriate supportive treatment.
Immediately interrupt the infusion and administer appropriate supportive treatment, as necessary. Restart the infusion only after all symptoms have resolved. When restarting, begin at half of the infusion rate at the time of onset of the infusion reaction. If this rate is tolerated, increase the rate as described in the infusion rate table.
Reduce the infusion rate to half the rate at the onset of the infusion reaction and maintain the reduced rate for at least 30 minutes. If the reduced rate is tolerated, increase the rate as described in the infusion rate table.
BRIUMVI must be prepared by a healthcare professional using aseptic technique.1 Prepare the solution for infusion as follows:
BRIUMVI should be a clear to opalescent, colorless to slightly yellow solution.

Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use the solution if discolored or if the solution contains discrete foreign particulate matter.
1
Prepare infusion bag for the first infusion (150 mg) using 1 vial (150 mg/6 mL) of BRIUMVI.
2
Withdraw 6 mL 0.9% NaCl injection, USP from the 250 mL infusion bag and discard.
3
Withdraw 6 mL BRIUMVI solution from the vial.
4
Add 6 mL (150 mg) BRIUMVI into the infusion bag containing 0.9% NaCl injection, USP.
5
Prepare infusion bag for second infusion (450 mg) and subsequent infusions (450 mg) using 3 vials (150 mg/6 mL) of BRIUMVI.
6
Withdraw 18 mL 0.9% NaCl injection, USP from the 250 mL infusion bag and discard.
7
Withdraw 18 mL BRIUMVI solution from the vials
(6 mL/vial).
8
Add 18 mL (450 mg) BRIUMVI into the infusion bag containing 0.9% NaCl injection, USP.
Mix diluted solution by gentle inversion. Do not shake.
NaCl=Sodium chloride
USP=United States Pharmacopeia
![]()
Prior to the start of the IV
infusion, the contents of the
infusion bag should be at
room temperature.
Administer the diluted infusion solution through a dedicated line.
![]()
Use the prepared infusion
solution immediately. If
the diluted solution is not
administered immediately,
store for up to:
24 hours in the refrigerator at
2°C to 8°C (36°F to 46°F)
If the diluted solution is stored refrigerated, allow it to equilibrate to room temperature prior to administration (~ 2 hours).
The diluted solution can be stored for an additional 8 hours at room temperature up to 25°C (77°F), which includes the equilibration time and infusion time.
Do not freeze.
![]()
No incompatibilities between
BRIUMVI and PVC or PO bags
and IV administration sets
have been observed.
IV=intravenous
PVC=polyvinyl chloride
PO=polyolefin
References: 1. BRIUMVI. Prescribing information. TG Therapeutics Inc; 2022. 2. Fox EJ, Steinman L, Hartung H-P, et al. Infusion-related reactions (IRRs) with ublituximab in patients with relapsing multiple sclerosis (RMS): post hoc analyses from the phase 3 ULTIMATE I and II studies. Presented at: 2022 American Academy of Neurology (AAN) Annual Meeting; April 2-7, 24-26, 2022; Seattle, WA.
Call 1-833-BRIUMVI (1-833-274-8684) to speak with a BRIUMVI Patient Support
Case Manager (Mon-Fri, 8 AM to 8 PM ET)
Are you a Healthcare Professional or a Patient or Care Partner?